A new analysis reveals that women’s risk of dying from cervical cancer is much higher than medical professionals originally thought, particularly among older and black women. Black women in America are dying from cervical cancer at a rate 77 percent higher than previously thought, while white women are dying at a rate 47 percent higher rate from the disease, according to a new study, published in the journal Cancer of the American Cancer Society on Monday (Jan 23). The situation among white women is still very serious, but significantly lower compared to black women.
“This shows that our disparities are even worse than we feared,” Dr. Kathleen Schmeler, an associate professor of gynecologic oncology at the University of Texas M. D. Anderson Cancer Center, told the New York Times. “We have screenings that are great, but many women in America are not getting them.”
After adjusting for hysterectomies (a surgical operation to remove part or all of the uterus), the journal Cancer found that the corrected mortality rate in black women was 10.1 per 100,000 women (between 2000 and 2012) instead of 5.7 and white women was 4.7 per 100,000 instead of 3.2 as previously thought. Previous estimates didn’t account for women whose cervixes were removed in hysterectomies, which eliminate the risk of developing the disease, according to the Johns Hopkins Bloomberg School of Public Health.
“Prior calculations did not account for hysterectomy because the same general method is used across all cancer statistics,” said Anne Rositch, assistant professor of epidemiology at Johns Hopkins and lead author of the study.
Meanwhile, many of those women who are dying from cervical cancer are above age of 65, a cut-off point where the cancer screening guidelines no longer recommend women with cervixes be regularly screened for cervical cancer. With routine screening, cervical cancer is preventable. Cervical cancer used to be the leading cause of cancer death for women in the U.S. the organization says. In the United States, 12,820 women are diagnosed with cervical cancer each year and 4,120 women die from the disease, according to the National Cancer Institute. However, the number of cases has significantly declined in the past 40 years due to proper screening.

“Although trends over time show that the racial disparity in cervical cancer mortality is closing, these data emphasize that it should remain a priority area,” said Dr. Rositch.
ABOUT CERVICAL CANCER?
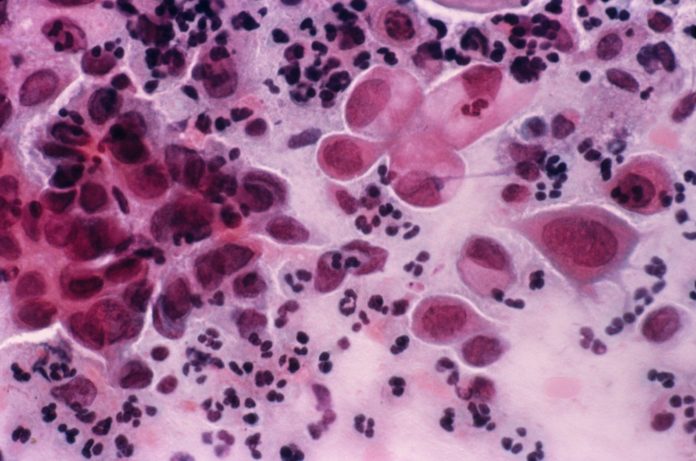
Cervical cancer is a cancer arising from the cervix, it occurs when abnormal cells on the cervix grow out of control. Cancer of the cervix – the neck of the womb – affects women of all ages, but it is most common in those women aged between 30 to 45 years.
CAUSE OF CERVICAL CANCER: –
Most cervical cancer is caused by a virus called HPV (human papilloma virus). You can get HPV by having sexual contact with someone who has it. There are many types of the HPV virus but not all types of HPV cause cervical cancer.
EARLY SYMPTOMS: –
1. Any unusual bleeding from the vagina, particularly after sex, or after the menopause when your periods have stopped.
2. Persistent vaginal discharge that is blood-stained or smells unpleasant.
3. Pain in the lower belly or pelvis.
WHY ARE MORE BLACK WOMEN DYING FROM CERVICAL CANCER?
Black women are more likely to have hysterectomies at a young age (in comparison to white women) because of their greater susceptibility to fibroids – benign masses in the uterus – which can cause cancerous symptoms.
IS CERVICAL CANCER PREVENTABLE?
Cervical cancer is highly preventable with vaccinations to prevent the HPV (human papilloma virus), which can cause the disease, are both available, according to the Centres for Disease Control and Prevention. Cervical cancer is also treatable when diagnosed early from screening tests. There is a vaccine for women age 26 and younger.
According to CDC recommendations, regular screening tests starting at age 21 are highly important by having a pap test every three years. Then, starting from the age of 30, they should have a pap test combined with a HPV test every five years to take all precautions.
Another part “Screening” is a huge part of effective cervical cancer diagnosis and prevention. The cell lining the surface of the cervix undergo a series of changes throughout a woman’s life, some of these cells might become cancerous. Screening for cervical cancer involves collecting a sample of these cells for analysis to check for any abnormal cells.
It is important to note that most abnormal results are caused by an infection or the presence of treatable precancerous cells, not by cancer.

1. Have regular Pap test screening (Pap test schedule is based on your age)
2. Quit smoking (Second-hand smoke/Passive smoking)
3. Get the HPV vaccine (The vaccines Cervarix, Gardasil, and Gardasil 9)
4. Reduce your risk of a sexually transmitted infection (STI)
“This is a preventable disease and women should not be getting it, let alone dying from it,” says Dr. Anne Rositch, PhD, MSPH, of the Johns Hopkins Bloomberg School of Public Health, and lead author of the research.